Attorney-Verified West Virginia Do Not Resuscitate Order Template
In the realm of healthcare decision-making, the West Virginia Do Not Resuscitate (DNR) Order form plays a crucial role for individuals who wish to communicate their preferences regarding life-sustaining treatments. This form serves as a legally binding document that outlines a patient's desire not to receive cardiopulmonary resuscitation (CPR) in the event of a cardiac arrest or respiratory failure. It is designed for patients who have a clear understanding of their medical condition and the implications of their choices. The DNR Order must be completed and signed by a physician, ensuring that the patient's wishes are respected and understood within the medical community. Importantly, the form also requires the patient or their legal representative to provide informed consent, reflecting a thoughtful consideration of the individual’s values and beliefs about end-of-life care. By completing this document, patients can alleviate the burden on their loved ones and healthcare providers during critical moments, ensuring that their preferences are honored. Understanding the intricacies of the West Virginia DNR Order form empowers individuals to take control of their healthcare decisions and fosters open conversations about end-of-life planning.
Some Other West Virginia Forms
Wv Lease - Fosters a rental environment founded on transparency and respect.
The Arizona Durable Power of Attorney form is a crucial legal document that enables individuals to appoint a trusted person to manage their financial and legal affairs, especially important in cases of incapacity. For further details and to obtain necessary documents, you can access the Durable Power of Attorney form, which is essential for safeguarding one's interests.
How to Get Financial Power of Attorney - Helps avoid court involvement in managing affairs.
Misconceptions
Understanding the West Virginia Do Not Resuscitate (DNR) Order form can be challenging, leading to several misconceptions. Here are eight common misunderstandings clarified.
- A DNR means no medical care at all. Many believe that a DNR order implies a complete withdrawal of all medical care. In reality, a DNR specifically addresses resuscitation efforts in case of cardiac or respiratory arrest, while other medical treatments can still be provided.
- Only terminally ill patients need a DNR. Some think that only those facing imminent death should consider a DNR. However, anyone with a serious medical condition or who wishes to avoid aggressive resuscitation can benefit from a DNR order.
- A DNR is permanent and cannot be changed. This misconception leads to fear about making a long-term decision. In fact, individuals can revoke or modify their DNR order at any time, as long as they are competent to do so.
- All healthcare providers must honor a DNR. While most healthcare professionals are trained to respect DNR orders, there may be specific circumstances or settings where a DNR might not be recognized. It’s essential to communicate your wishes clearly to all involved in your care.
- A DNR is only for older adults. Many associate DNR orders with elderly patients, but younger individuals with serious health issues may also choose to establish a DNR. Age does not determine the need for such an order.
- Having a DNR means you are giving up on life. This misconception can create stigma around DNR orders. In truth, a DNR reflects a personal choice about the type of care one desires, emphasizing quality of life over aggressive interventions.
- You need a lawyer to complete a DNR. Some believe that legal assistance is necessary to fill out a DNR form. In West Virginia, individuals can complete the form on their own, provided they understand its implications and requirements.
- A DNR order is only valid in hospitals. While many think DNR orders apply only within hospital settings, they are valid in various healthcare environments, including at home or in nursing facilities, as long as the proper documentation is in place.
Understanding these misconceptions can help individuals make informed decisions regarding their healthcare preferences and ensure their wishes are respected.
West Virginia Do Not Resuscitate Order: Usage Instruction
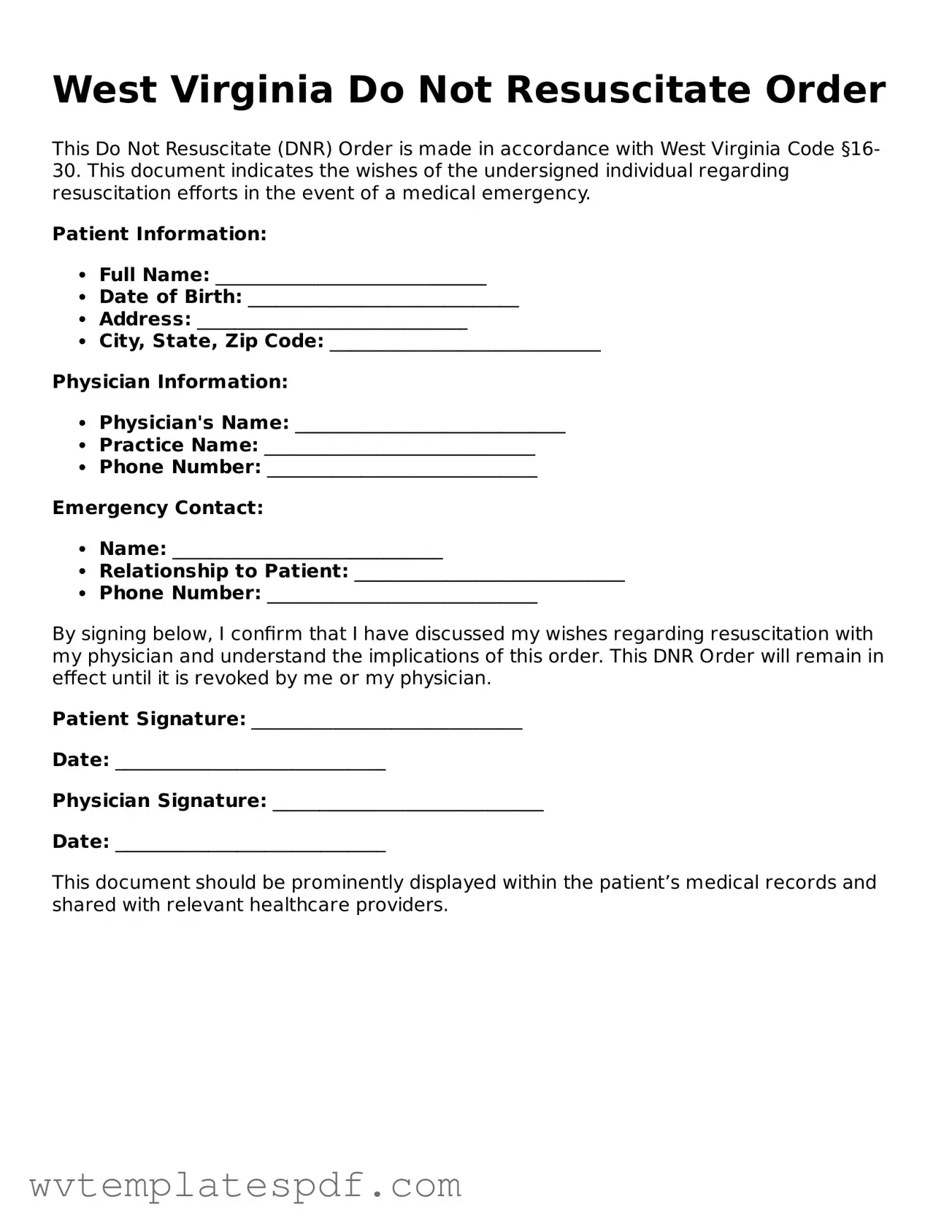
Filling out the West Virginia Do Not Resuscitate Order form is an important step in expressing your healthcare preferences. This process ensures that your wishes regarding resuscitation efforts are clearly communicated to medical professionals. Follow these steps carefully to complete the form accurately.
- Obtain the West Virginia Do Not Resuscitate Order form. You can find it online or request a copy from your healthcare provider.
- Begin by filling in your full name, date of birth, and address at the top of the form. This information helps identify you clearly.
- Next, indicate whether you are completing this form for yourself or if it is being completed on behalf of someone else. If it is for someone else, include their name and relationship to you.
- In the designated section, clearly state your wishes regarding resuscitation. Make sure to read the options carefully before making a selection.
- Sign and date the form. Your signature confirms that you understand the contents of the document and agree with the decisions made.
- Have a witness sign the form. This witness should not be a family member and must be over the age of 18. Their signature adds validity to your wishes.
- Make copies of the completed form. Keep one for your records and provide copies to your healthcare provider and any family members involved in your care.
Once the form is completed, it is crucial to ensure that all relevant parties are aware of your decisions. Regularly review your choices and update the form as necessary, especially if your health status changes or if you have new preferences.
Similar forms
- Advance Healthcare Directive: This document allows individuals to outline their healthcare preferences in advance. Like a Do Not Resuscitate Order, it can specify what types of medical interventions a person does or does not want in critical situations.
- Living Will: A living will is similar to an Advance Healthcare Directive. It provides specific instructions regarding medical treatment preferences, particularly in end-of-life scenarios. Both documents aim to communicate a person's wishes when they cannot speak for themselves.
- Last Will and Testament: To ensure your final wishes are honored, consider the important last will and testament form details, which guide you in designating asset distribution and care for your loved ones.
- Healthcare Power of Attorney: This document designates an individual to make healthcare decisions on behalf of another person. While a Do Not Resuscitate Order is a specific directive, the Healthcare Power of Attorney grants broader authority to manage medical care according to the individual's wishes.
- Physician Orders for Life-Sustaining Treatment (POLST): A POLST form is similar in that it provides specific medical orders regarding treatment preferences. Unlike a Do Not Resuscitate Order, which primarily focuses on resuscitation, POLST encompasses a wider range of medical interventions.
- Medical Order for Life-Sustaining Treatment (MOLST): This document serves a similar purpose to POLST. It is designed to communicate a patient's preferences for life-sustaining treatments. Both documents are intended to ensure that medical personnel follow the patient's wishes in emergencies.
Documents used along the form
The West Virginia Do Not Resuscitate (DNR) Order form is an essential document for individuals who wish to communicate their preferences regarding resuscitation efforts in the event of a medical emergency. Alongside this form, there are several other important documents that can help clarify a person's healthcare wishes. Below are four commonly used forms that complement the DNR Order.
- Advance Directive: This document allows individuals to outline their preferences for medical treatment in situations where they may be unable to communicate their wishes. It can include instructions regarding life-sustaining treatments and appoint a healthcare proxy to make decisions on their behalf.
- Residential Lease Agreement: This document outlines the terms of rental agreements, ensuring both landlords and tenants are clear on their rights and responsibilities. For a comprehensive template, you can refer to Arizona PDFs.
- Healthcare Power of Attorney: This legal document designates a specific person to make healthcare decisions for an individual if they become incapacitated. It ensures that someone trusted is responsible for making choices that align with the individual's values and preferences.
- Living Will: A living will is a type of advance directive that specifically addresses an individual's wishes regarding end-of-life care. It provides guidance on the types of medical treatments one would or would not want, such as mechanical ventilation or feeding tubes.
- Physician Orders for Life-Sustaining Treatment (POLST): This form is intended for individuals with serious illnesses. It translates a patient’s treatment preferences into actionable medical orders, ensuring that healthcare providers follow the patient's wishes regarding life-sustaining treatments.
Each of these documents plays a crucial role in ensuring that healthcare providers and family members understand and respect an individual's wishes regarding medical treatment. It is important for individuals to have these conversations and complete the necessary paperwork to ensure their preferences are honored in critical situations.
Common mistakes
Filling out a Do Not Resuscitate (DNR) Order form in West Virginia is a serious task that requires careful attention. Unfortunately, many individuals make common mistakes that can lead to confusion or complications in critical moments. Understanding these pitfalls can help ensure that your wishes are clearly communicated.
One frequent error is not including all required signatures. The DNR form must be signed by both the patient and their physician. If either signature is missing, healthcare providers may not honor the order. Always double-check that all necessary parties have signed before submitting the document.
Another mistake involves failing to clearly identify the patient. It’s essential to provide accurate personal information, including the full name, date of birth, and any other identifying details. If the information is vague or incorrect, it could lead to misunderstandings about whose wishes are being respected.
Some individuals also overlook the importance of discussing the DNR order with family members. This conversation is crucial for ensuring that loved ones understand the patient’s wishes. Without this discussion, family members may be caught off guard during a medical emergency, leading to confusion and potential conflict.
Moreover, people sometimes forget to review and update their DNR orders. Life circumstances can change, and it’s important to revisit the document regularly. If a patient’s health status or preferences change, the DNR order should reflect those updates. Neglecting this can result in a document that no longer aligns with the patient’s current wishes.
Lastly, many individuals fail to keep copies of the DNR order in accessible locations. It’s not enough to fill out the form; having copies on hand in various settings—such as at home, with family members, and in medical records—ensures that healthcare providers can easily access the order when needed. This simple step can make a significant difference in honoring the patient’s wishes during emergencies.
Key takeaways
Here are key takeaways about filling out and using the West Virginia Do Not Resuscitate Order form:
- The form must be completed by a licensed physician.
- It is essential for the patient or their legal representative to provide informed consent.
- The order should be clearly documented in the patient's medical record.
- Patients can revoke the order at any time, verbally or in writing.
- Healthcare providers must comply with the order once it is properly executed.
- The form should be readily accessible in emergency situations.
- It is advisable to discuss the order with family members and caregivers.
- Regular reviews of the order are recommended to ensure it reflects the patient's current wishes.